Dry Eye Clinic
DRY EYE
Dry eye syndrome (DES) is a lack of sufficient lubrication and moisture on the front surface of the eye and affects hundreds of millions of people. Our tears help maintain the health of the cornea as well as provide clear vision. Dry eye syndrome is a multifactorial condition characterized by loss of homeostasis on the ocular surface. It can be caused by decreased tear production, excessive tear evaporation, and/or inflammation. Most cases of dry eye syndrome have been shown to be a combination of these as well as other environmental factors.
DRY EYE SYMPTOMS
The most common symptoms are burning, scratchiness, redness, gritty/sandy sensation, and an overall dryness feeling. These symptoms alone can be enough to diagnose dry eye syndrome. Other symptoms include blurred vision, tired eyes (especially on a computer), and contact lens intolerance. It may seem paradoxical, but dry eye syndrome can cause watery eyes. This is because dryness on the eye’s surface sometimes will overstimulate production of the watery component of your tears as a protective mechanism.
WHO IS AT GREATEST RISK?
Dry eye syndrome is the most common eye disorder, affecting 1 in 5 people. It is more common with age and as body hormone changes occur, especially in post-menopausal women. Medications taken by mouth can cause dry eyes, including antihistamines, blood pressure medications, decongestants, and antidepressants. Complaints of dry eyes are particularly common in patients with certain medical conditions such as rosacea, rheumatoid arthritis, thyroid disease, and certain autoimmune conditions like lupus. The most severe form of DES is related to a condition known as Sjogren’s Syndrome. This condition affects several million people throughout the world and patients experience dry mouth/throat in addition to dry eyes. Many patients that have had refractive surgery like LASIK are subsequently dealing with dry eye syndrome. Environmental factors such as computer use, contact lens wear, or simply being in a high air flow environment can all increase risk.
DRY EYE TESTING
There are various tests performed to determine the presence and type of DES, but the most important is conducting a careful case history to uncover dry eye symptoms from the patient’s perspective. In our clinic a standardized questionnaire is used to determine the severity of dryness symptoms. At Vision Care Associates we have sophisticated instrumentation to test various ocular surface parameters. Here are a few that are important:
-Tear osmolarity: A small sample is taken of your tears and the “lab on a chip” can measure the salt content of the tear film. This is an objective measurement of the quality of a person’s tears. A score of 300 or lower is considered normal.
https://www.youtube.com/watch?v=QytxRb8mPmo&authuser=0

-Tear evaporation time: Our high-resolution video measures how long tears cover the ocular surface after each blink. Normal tear functioning will measure 8 seconds or more before tears dissipate.
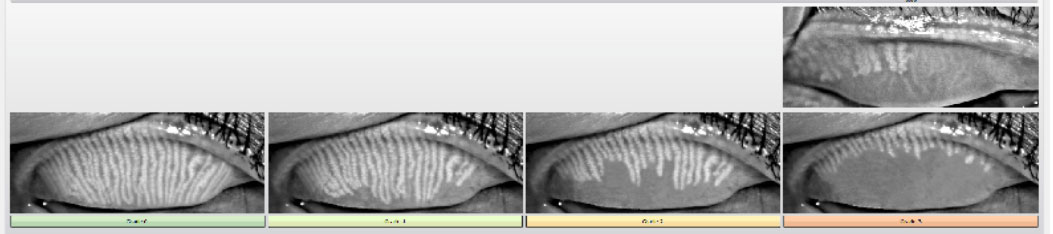
-Meibography- An infrared camera shows the condition of the meibomian glands on the eyelids. These glands are important as they produce the oil that holds our tears on the eye. One large study found that 86% of dry eyes is caused by disfunction of the meibomian glands.
-Tear Lake: Measure of the overall volume of tears.
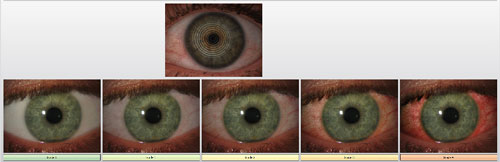
-Redness: Our high-resolution camera takes an up-close photo to measure the engorgement of the blood vessels on the “whites” of the eye. This is a barometer for the amount of inflammation on the ocular surface.
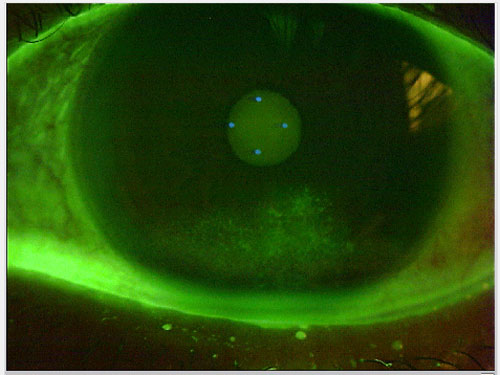
-Biomicroscope evaluation: Investigation of the cornea, tear film and eyelid margins under the microscope. This is sometimes done by instilling an orange water dye.
DRY EYE TREATMENT
Dry eye syndrome is a chronic (and often progressive) disease for which there is no permanent cure. It is important to determine the underlying cause so a targeted treatment plan can be recommended. The goal of treatment is to restore homeostasis of the ocular surface and tear film. While certain treatments may be specifically indicated for one particular aspect of an individual’s condition, multiple therapies may be recommended due to the multifactorial nature of the disease and the adjunctive benefits of therapies. Mild dry eyes can sometimes be managed with non-prescription artificial tears. Since there are an overwhelming number of artificial tears available it is prudent to use the formulation that is designed for each patient’s specific type of dry eyes. We often recommend preservative-free artificial tears as they can be used more frequently and with no worry of toxic side effects from a preservative. Lubricating gels and ointments may also be recommended, but are best used at night as they can blur your vision. Restasis, Xiidra, and Cequa are other excellent treatment options. They are all prescription eye drops that have been shown to reduce inflammation and subsequently cause better tear production and tear quality. Punctal plugs can be a great treatment option once inflammation is well controlled. With this treatment small silicone plugs are gently placed into the tear ducts to block the tears from draining away and allowing longer contact time on the ocular surface. Oral supplements such as Omega-3 fatty acids can improve meibomian gland function and thus improve the tear film. Autologous serum eye drops are a newer treatment option that has worked well for many of our severe dry eye patients. It is made out of blood drawn from the patient. The blood is centrifuged; the serum is drawn off and then packaged as an eye drop. The benefit of this modality is the biochemical properties of blood serum are very similar to that of the tear film. The components have an anti-inflammatory effect as well as providing essential nutrients to the cornea and tear film.
The newest treatment available for dry eyes is Intense Pulsed Light (IPL). This technology has been used for decades by doctors to treat a variety of skin conditions including rosacea, vascular and pigmented skin lesions, and even skin rejuvenation. IPL works by penetrating the skin and targeting abnormal blood vessels that are thought to be the root cause of oil gland inflammation on the eyelids. The dry eye protocol for IPL can treat your skin and eyelid inflammation while improving overall skin appearance. Treatments are completed in 4 separate sessions typically scheduled 3-4 weeks apart. Most patients experience a benefit after the second or third treatment. Individual maintenance treatments can be performed every 6-12 months if needed.


If you or someone you know is experiencing dry eye symptoms, call to schedule a consultation today. Our doctors have experience and expertise when it comes to dry eye syndrome. The sooner proper treatment is applied to the ocular surface, the better the outcome.
